What is Newborn Pulmonary Hypertension?
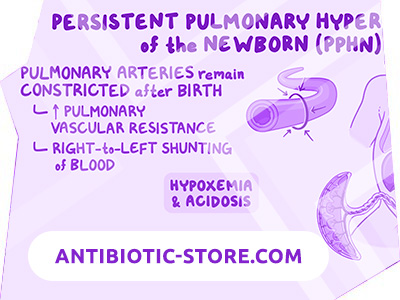
Persistent pulmonary hypertension in newborns is a persistence or return to a state of constriction of the arterioles of the lungs, which reduces blood flow in the baby’s lungs and causes a right-left blood discharge.
Forms of pulmonary hypertension in newborns:
- primary
- secondary
Primary pulmonary hypertension is diagnosed in infants who have recently been born and who do not have vivid symptoms and radiological evidence of lung pathology. After birth, the development of persistent hypoxemia soon occurs. But the level of PaCO 2 is normal or slightly reduced. The cause may be a primary dysfunction of the mechanisms of pulmonary vasodilation.
Secondary pulmonary hypertension in a newborn occurs in severe, mainly parenchymal, lung diseases. This complicates the course of the disease and worsens the prognosis. Pulmonary hypertension in children often occurs along with meconium aspiration syndrome, respiratory distress syndrome, pneumonia, diaphragmatic hernias, and other forms of PH. In such cases, pulmonary vasoconstriction is associated with hypoxia.
Primary pulmonary hypertension in newborns occurs in 1-3 cases out of 1 thousand. The diagnosis is typical for long-term and normally full-term children. With caesarean section, LHN is 5 times more likely than normal delivery during childbirth. Pulmonary hypertension is rare in premature infants – premature among the total number of children with this diagnosis make up only 15-35%.
Smooth muscles surrounding pulmonary arterioles develop only at the 28th week and later at the end of gestation. Therefore, pulmonary hypertension is not a problem that is relevant for prematurely born children. the structure and function of the vessels of the lungs of the embryo change when it grows. Gas exchange in the fetus occurs due to the placenta, and not due to the lungs. Less than 10% of the mixed blood that has left the ventricle circulates through the pulmonary vascular system, and a large percentage of the blood from the right ventricle enters the arterial duct, enters the aorta, from where it passes through the ascending aorta to the upper limbs and head.
Causes of Pulmonary Hypertension in Newborns
Persistent pulmonary hypertension in newborns occurs in many cases due to perinatal hypoxia or asphyxiation. Often, meconium staining of the amniotic fluid occurs, or a history of meconium is fixed in the trachea. Hypoxia provokes the return or persistence of severe constriction of arterioles in the lungs, which is normal in the fetus.
Among the additional reasons, premature closure of the ductus arteriosus or oval foramen is distinguished, which causes an increase in pulmonary blood flow in the fetus. The reason may be taking a pregnant non-steroidal anti-inflammatory drug. Also, the cause may be polycythemia – a disease in which there is a violation of blood flow.
A common cause of the disease is a congenital diaphragmatic hernia. With this diagnosis, the left lung is very hypoplastic, because a large amount of blood goes to the right lung. Another reason is neonatal sepsis. Whatever the cause of pulmonary hypertension in newborns, increased pressure in the pulmonary artery causes abnormal development and hypertrophy of the smooth muscles of the walls of the pulmonary arteries of small caliber and arterioles, as well as a right-left blood discharge through the arterial duct or oval window, which leads to persistent systemic hypoxemia .
Pathogenesis during Pulmonary Hypertension of the Newborn
The function of the endothelium, the inner lining of the vessels, is impaired. The excessive production of vasoconstrictor substances begins, and the formation of the formation of vasodilating substances, on the contrary, decreases. An inflammatory process occurs at the level of the capillary endothelium, thrombosis develops in a certain area. In response to hypoxia, a spasm of the pulmonary capillaries occurs – the oxygen content decreases. In pathogenesis, the overgrowth of the muscle components of the vascular wall of the pulmonary capillaries is important.
The above described changes cause a narrowing of the lumen of the vessels of the lungs. Vascular resistance also increases and pressure in the pulmonary artery system increases. This leads to the fact that the load on the heart becomes much greater. The result is heart failure in a newborn.
Symptoms of Newborn Pulmonary Hypertension
The main symptoms are retraction of the malleable places of the chest, tachypnea, decreased oxygen saturation, severe cyanosis. Oxygen therapy does not give effective results. In infants with a right-left shunt through an open arterial flow, oxygenation in the right brachial artery is higher than in the descending aorta. For this reason, cyanosis can be uneven. That is, the oxygen saturation on the legs is about five percent lower than on the upper right arm.
Diagnosis of Pulmonary Hypertension in Newborns
Newborn pulmonary hypertension is suspected in babies who are born on time or later than the appointed time and who have arterial hypoxemia and / or cyanosis. An appropriate medical history also helps in the diagnosis. The child does not have an increase in oxygen saturation while breathing 100% oxygen, which is an important diagnostic sign.
Methods for confirming the diagnosis are echocardiography with dopplerography. They confirm increased pressure in the pulmonary artery. They are also necessary to exclude congenital heart disease, which can be confused with the disease in question. X-ray shows that the pulmonary fields are normal or there are changes that are adequate to the cause of the disease:
- congenital diaphragmatic hernia
- neonatal pneumonia
- meconium aspiration syndrome
Treatment of Pulmonary Hypertension in the Newborn
In children with a diagnosis of persistent pulmonary hypertension of the newborn, hearing impairment, developmental delay, and functional impairment occur. Oxygen therapy should be started slowly so that the disease does not develop further. Oxygen is supplied using a bag and mask or a mechanical ventilator. High-frequency oscillatory ventilation allows you to straighten and ventilate the lung, barotrauma along with this is minimized.
When a child breathes in, nitric oxide relaxes the smooth muscles of blood vessels and dilates the arterioles of the lungs. Because blood flow in the lungs increases, oxygenation improves in about half of patients quickly. The initial dose is 20 ppm, in the future it needs to be reduced in order to maintain the effect.
In severe hypoxic respiratory failure, a method such as extracorporeal membrane oxygenation can be used. The oxygenation index for this form of the disease is above 35-40, despite the maximum respiratory support. It is necessary to maintain normal levels of electrolytes, fluids, calcium, glucose. The child should be in a room with optimal temperature. They give him antibiotics until they get the results of the sowing, when it will be possible to understand whether this sepsis or not.